Meningiomas are often benign tumors arising from the coverings of the brain and spinal cord. They represent about one-third of all primary brain tumors and occur most frequently in middle-aged women. Meningiomas usually grow inward, causing pressure on the brain, spinal cord, or eye. They also can grow outward toward the skull, causing it to thicken. Most meningiomas are benign (non-cancerous), slow-growing tumors. Some contain sacs of fluid (cysts), mineral deposits (calcifications), or tightly packed bunches of blood vessels. Meningiomas are graded 1, 2, or 3. A higher grade signifies that the meningioma is more aggressive.
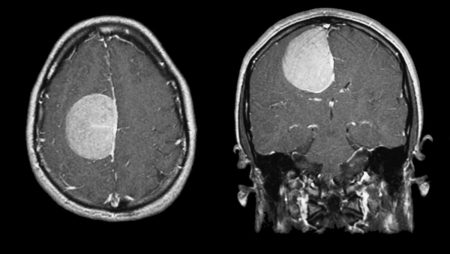
MRI of a meningioma.
Location
Although meningiomas are referred to as brain tumors, they do not grow from brain tissue. They arise from the meninges, which are three thin layers of tissue covering the brain and spinal cord. These tumors are most often found near the top and the outer curve of the brain. Meningiomas may also form at the base of the skull.
Have you or a loved one been diagnosed with Meningioma?
Start here.
We’ve put together a few first steps to help you navigate a Meningioma diagnosis. This free educational booklet has what you need to make sense of your diagnosis and treatment, and tips for moving forward.
Symptoms
Meningiomas usually grow slowly and may reach a large size before interfering with the normal functions of the brain. The resulting symptoms depend on the location of the tumor within the brain. Headache and weakness in an arm or leg are the most common symptoms. However, seizures, personality changes, and/or visual problems may also occur.
Treatment
Meningiomas are often found incidentally on brain scans ordered for other reasons (e.g., head trauma). For small, asymptomatic meningiomas active surveillance is sometimes the best course of action. Scans (e.g. MRI, CT, DOTATATE PET) are performed at regular intervals to assess growth, and any new or unusual symptoms should be reported to your doctor right away.
Surgery is the primary treatment for meningiomas. Radiation therapy or stereotactic radiosurgery (SRS) may be used to treat tumors that cannot be safely removed with surgery or residual tumor that could not be completely removed during surgery. Radiation therapy or SRS can also be used to treat malignant (cancerous) tumors or recurrent tumors. Drug therapy may be used to treat meningiomas that cannot be removed surgically, when radiation therapy is contraindicated, or if the meningioma recurs or comes back. Drug therapy can include targeted therapy specific to a meningioma’s mutation by pill, infusion, or injection.
Prognosis
Prognosis means a prediction of outcome. This information is usually based on information gathered from groups of people with the same disease. It is important to remember these statistics are not individualized.
The 5-year relative survival rates for benign (non-cancerous) meningioma by age group are as follows:
- Children (0-14): 96.5%
- Adolescents and Young Adults (15-39): 97.2%
- Adults (40+): 87.6%
The 5-year relative survival rates for malignant (cancerous) meningioma by age group are as follows:
- Children (0-14): 79.6%
- Adolescents and Young Adults (15-39): 84.4%
- Adults (40+): 65.1%
Incidence
Meningiomas account for about one-third of all primary brain tumors. They occur about twice as often in women as in men.
Approximately 83% of meningiomas are Grade 1, 15% are Grade 2, and 2% are Grade 3.
Age Distribution
Meningioma can occur in people of all ages but are most likely to be found in older adults (median age of 65). Rarely are meningiomas found in children.
Risk Factors
Although the exact cause of meningioma is not known, it has been associated with age and radiation exposure. Higher risk occurs with greater levels of exposure to radiation at a younger age. Some genetic syndromes carry an increased risk for meningioma, including neurofibromatosis type 2, schwannomatosis, and Gorlin syndrome. There is some evidence of an association of estrogen and progesterone hormones with increased risk for meningiomas, which is suggested by the increased incidence in women compared to men.in some meningiomas, some evidence shows increased risk associated with hormone use and obesity. There is no conclusive evidence that head trauma or cell phone use increases the risk for meningioma.
Molecular Profile
Molecular profiling is the detection of specific genes, proteins, or other molecules in a tumor. This information helps confirm tumor diagnosis, inform treatment options, and predict prognosis.
The most described genetic alteration is the loss of chromosome 22, normally involved in suppressing tumor growth. It is seen in approximately 50% of patients with mutations in the neurofibromatosis type 2 (NF-2) gene. Multiple meningiomas occur in 5–15% of patients, particularly those with NF-2. Meningiomas also frequently have extra copies of the platelet-derived growth factor (PDFGR) and epidermal growth factor receptors (EGFR), which may contribute to the growth of these tumors. New evidence shows that meningiomas with certain mutations (TERT and CDKN2A/B homozygous loss) are more aggressive and are Grade 3 meningiomas. Most meningiomas express SSTR2, a receptor found on the surface of meningioma cells. SSTR2 can be detected by DOTATATE-PET and is the target for some drug therapies.
Content last reviewed:
June 2024 by Carlen Yuen, MD and Jennifer Yu, MD, PhD



